>
Introduction
In this article we presents an overview of how testosterone is stimulated in the body, shows how calorie balance affects T production, and discusses how dietary protein intake affects circulating T levels.
The HPT Axis
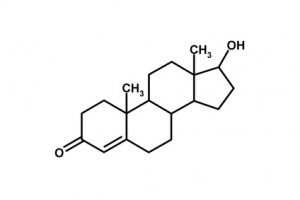
An article on the effects of diet on hormones would be incomplete without a basic overview of the relationships between the organs and hormones of the axis. The term axis simply refers to the pathway in question. The glands of this pathway include the hypothalamus, pituitary, and testes. The sequence of events culminating with the production and/or release of T begins at the hypothalamus. Here specialized nerve cells release a hormone called gonadotropin-releasing hormone (GnRH). GnRH is a decapeptide (chain of ten amino acids) that travels by direct blood vessel connections to the anterior pituitary where it stimulates the release of luteinizing hormone (LH) (1). LH is then secreted into the blood where it attaches to receptors on the Leydig cells of the testes. This induces activity of an enzyme, P-450scc, referred to as the cholesterol-side-chain-cleavage enzyme (1). Through a series of five enzymatic steps, cholesterol is converted into T.
The body regulates the circulating blood levels of T via several mechanisms. Once in the blood, about 44% of T is bound to a protein called either sex-hormone-binding-globulin (SHBG) or testosterone-binding globulin (TeBG), to indicate the greater affinity for T over estradiol (E2, an estrogen). About 54% of T is bound by albumin and other proteins, leaving 2% to circulate unbound to any protein. This unbound T is termed free testosterone (fT) (1). It is currently believed that only the fT or albumin bound T are truly available to interact with the tissues of the body. The significance of this point will be elaborated upon later in reviews of the data from different studies. Of the T that is available to interact with tissues, some of it binds to steroid receptors. In most tissues, like skeletal muscle, it will directly stimulate protein synthesis. In some tissues, like the brain and fat cells, it can be converted into E2 via the aromatase enzyme. In other tissues, like the prostate gland, it can be converted into dihydrotestosterone (DHT) via the 5-alpha-reductase enzyme. T either directly or through conversion to E2 or DHT can inhibit its own future production. The conversion to E2 or DHT can take place both in the brain and various other tissues. E2 and T exert stronger inhibitory effects than DHT on T production. This process is called negative-feedback inhibition. This is the reason why the use of steroids, enzyme inhibitors, and prohormones are far from perfect in their effects on increasing T levels. Because it is a dynamic process, as T levels elevate in the blood, a corresponding increase in inhibitory signals occurs. This results in the body making less T. The opposite occurs when T levels decrease. This is a basic overview and presented in a simplistic static fashion. The body is a highly dynamic organism and many factors come into play to help regulate this process. This point is made to illustrate the confounding problem that occurs when trying to increase circulating levels of androgens.
Effects of Calorie Intake on Testosterone
Every minute of the day, someone makes a decision to lose weight. Dieting by means of restricting calories, while not always successful, is practiced frequently. There are some people who believe that fasting (or what we call planned starvation) is a necessary method for cleaning the body of wastes. What effects does depriving the body of calories have on endocrine responses within the HPT axis? As you may have already guessed, it screws things up. Fasting for 5 days can lower LH, T, and fT by 30-50% (2). What appears to happen is that as the body becomes deprived of energy, less GnRH is released from the hypothalamus. This, in turn, leads to a weaker signal to release LH. While the pattern of LH release remains the same, the amount of LH released at each interval decreases, meaning your body is giving weaker signals to stimulate T. In addition, research on fasting in rats indicates that testicular enzymes involved in synthesizing T decrease in function (3). This means that even if enough LH reaches the testes, they still cannot produce normal amounts of T. The decrease in T can be a contributing factor to the loss in lean body mass that occurs with fasting. Of course, this is contrary to what most of us want to do in the quest to get bigger and stronger. However, many elite athletes have learned how to apply fasting to their contest preparation. Fasting before a drug test is a common practice when on anabolic-androgenic steroids because it helps prevent testing positive. But before you run out and load up on some “juice” and think you’ll beat a drug test just by fasting, keep in mind that this method is not always reliable, nor does it work when you have foreign metabolites in the body.
One of the common problems when dieting is holding onto all that hard earned muscle. Severe calorie restriction, whether from reduced food intake or imposed by excessive exercise, lowers testosterone (4). While there are no numbers written in stone, a decrease in calories by 15% does not lower T levels (5). This may serve as one factor to consider when planning out a diet strategy. If you cut back too much on your calories, then you risk lowering your T, which can cause you to say goodbye to some of your muscle. The good news is that when refeeding resumes and calorie intake equals calorie expenditure, in most cases, T levels will rise back to normal. The bad news is that if you are engaging in chronic high volume endurance exercise, even extra calories won’t help raise your T levels back to normal.
When male subjects are overfed in an attempt to induce weight gain, there tends to be a decrease in T levels as upper body fat increases (6). It may be wise, therefore, to limit calorie intakes to less than 1000 Calories (kilocalories) above energy requirements. From reviewing the literature, it seems that with large short-term increases in body fat and small chronic increases, T levels go down. Perhaps this is due to an inverse relationship between T and insulin and/or the aromatase enzyme. It is clear that with excessive body fat, aromatase activity in fat cells increases, thus more of T is converted into an estrogen called estradiol (E2). The issue with insulin is far more complicated and not really clear. Some research has shown insulin to regulate T in a positive fashion (7), while carbohydrate and protein liquid meals, which elevate insulin, have been shown to decrease T in resistance- trained males (8,9). This may be due to an increased uptake by tissues, like skeletal muscle, increased excretion of T in the urine, or decreased responsiveness of the testes to produce T.
While not related to caloric intake, hydration and sleep status are also important. A reduction of 3.8% in body weight due to dehydration did not affect T levels during mild exercise (10). But, don’t take any chances with hydration. Drink plenty of water every day at the rate of 30 cc per kilogram of body weight (or roughly one ounce for every two pounds). Get plenty of sleep, as disturbances in sleep and light/dark cycles can decrease T by almost 50% (11). Of course, no one ever gets enough sleep!
Dietary Protein Intake & Testosterone
The direct impact of protein by itself on T levels has not been well studied in humans. Some research on high protein diets deals with the effects on very obese people and weight loss. While this may not seem applicable to you, read on and we will put it together for you. In obese men, feeding 600 calories a day with 400 calories from protein (50 grams of beef protein and 50 grams of casein) induces lower levels of T than fasting does (12). Normally, when the kidneys filter T out of the blood, some T gets reabsorbed back out of the kidneys into the blood. The researchers stated that the additional protein in the diet generated more ketones. They concluded that the ketones were filtered out of the blood by the kidneys and were reabsorbed back into circulation preferentially over T. While most people reading this may not be obese, higher protein diets are definitely in vogue, more so for bodybuilders and powerlifters than other groups of athletes. The potential exists that if a ketogenic diet like the Atkins Diet or a cyclical ketogenic diet like the Anabolic Diet or Bodyopus is followed, than urinary excretion of T will be greater during the ketogenic phase of the diet.
It is known that protein in the diet can influence the metabolism of a variety of chemicals. Through a series of experiments, it was demonstrated that various foods could influence the metabolism of drugs in the body (13). Vegetables like cabbage and brussel sprouts were found to alter the function of specific liver enzymes. This, in turn, could change the half-life of a drug in the blood. Given the variety of diets that people follow and the variety of prescription medications and over-the-counter drugs people take, the logical progression was to look at how altering the macronutrient composition of the diet affected drug metabolism. It turns out that a higher ratio protein diet, a diet with more calories from protein than carbohydrates or fat, metabolizes some drugs faster, thus decreasing the clearance time of the drug. Since diet can affect drug metabolism, perhaps it could affect liver enzymes involved in the metabolism of endogenous steroids. Sure enough, it was found that a high ratio protein diet decreased the reduction of T (14). Reducing the reduction of T could mean a potential decrease in DHT and/or androsterone in the blood, which is good by most accounts. However, DHT levels were not measured and, more importantly, urinary T excretion increased, although it was not statistically significant. These subjects were not in ketosis, so perhaps ketones do not increase T excretion rates. Regardless of the exact mechanism, there is sufficient evidence in the literature that when protein intake exceeds carbohydrate intake, T clearance increases by excretion in the urine.
A cross over design study used seven normal men from 23-43 years of age and compared a high protein diet to a high carbohydrate diet (15). This study has been referenced many times and cited as proof that high protein diets lower total T levels in the blood. The high carbohydrate diet from this study will be covered in Part II. The high protein diet consisted of 44% protein, 35% carbohydrate, and 21% fat and supplied between 2400 and 2500 kilocalories per day (kcals/d). Let’s assume it was an even 2450 kcals/d. The men also had bodyweights that ranged from 64-72 kg. If we assume the mean was 68 kg, then this would give us an average body weight of about 150 pounds. This means these guys were eating [(2450 kcals/d times .44) (divide by 4)] 270 grams (g) of protein, [(2450 x.350 /4] 215 g of carbohydrates (CHO) and [(2450 x .21) /9] 58 g of fat per day.
However, total T is not that big of a deal. The more important measure is the bioactive fraction of T. (Earlier in the overview of the HPT Axis, it was mentioned that SHBG-bound T is not considered bioactive, while the other fractions of T are). While subjects followed the high protein diet, their total T levels were 28% lower than on the higher CHO diet (15). This is important because T decreased in all seven subjects, although the magnitudes of the decrease ranged from 10 to 93%. For the same seven subjects, their SHBG levels decreased about 39% with a range from 19 to 64%. Looking at this data gives the impression that the actual bioactivity of T was higher while the subjects were on a high protein diet. SHBG-bound T and fT were not measured, so it is not known for sure. On the surface it appears that a mean decrease of 39% in the SHBG values and only a 28% in the T would leave more T available for binding to tissues. However, if we calculate out the actual changes in the hormones using the data from the study, we see something different. The mean and standard error (M±SE) for T was 371 ± 23 ng/dL. The currently used units in clinical chemistry are nmol/L. Multiplying the mean T by the conversion factor of 0.0347 gives us about 12.9 ± .8 nmol/L. The M±SE SHBG was 23.4 ± 1.6 nmol/L. If we assume that the amount of T bound to SHBG averages 44%, then .44 x 12.9 ± .8 nmol/L gives us 5.7 ± .4 nmol/L of T bound to SHBG. That leaves 7.2 ± .4 nmol/L of T to interact with tissues in the body. However, we don’t know from the data if the amount of SHBG bound T decreased below or increased above the normal 44%, in which case there would be more or less T available to interact with tissues.
From work by the same group of researchers using the exact same diet (but different subjects) we see that the ratio of 5a – reduction to 5b – reduction (5a /5b ) of T is reduced by about 50%, with the decrease being attributed to lower rates of 5a – reduction (14). The T values that have been used thus far (15) already reflect any changes in altered T metabolism, so the conversion to a 5a – reduced hormone (ie androsterone) is accounted for at this point. Note that even though there is a decrease in 5a – reduced hormone production, it does not show up as increased T levels. The decrease in androsterone probably shows up in small, but statistically insignificant increases in other metabolites of T (they were statistically insignificant perhaps due to the small sample size). Another interesting aspect is that there is an increase in the oxidation of estradiol on the higher protein diet by about 14-15% (14). Unfortunately estradiol levels were not measured in this paper. This could have given us clues as to the mechanism by which higher protein diets lower T (ie increased negative feedback on T levels via estradiol). At this point, this is only one study and it is still difficult to come to any final conclusions. However, if this is what really happens, then a high-protein diet may actually lower the anabolic actions of T in the body. Unfortunately, this has not been verified through laboratory research and is just a theory at this point. Perhaps the decrease in T is a result of increased excretion in the urine either as T or a sulfated metabolite, or increased conversion to estradiol and oxidation by the liver.
source: thinkmuscle.com
Tags: Calories and Protein, Diet, Testosterone
This entry was posted
on Sunday, May 16th, 2010 at 4:04 pm and is filed under HEALTH PUBLICATIONS.
You can follow any responses to this entry through the RSS 2.0 feed.
You can leave a response, or trackback from your own site.